Anatomy in Cutaneous Surgery
Skin Tension Lines
Skin tension lines (STLs) are the result of a complex interaction between internal and external factors involving the skin. The intrinsic framework, which consists of elastin and collagen, progressively loosens with age. Their interaction with the muscles of facial expression leads to the development of STLs. Generally, STLs are perpendicular to the underlying muscles of the face. Aging, particularly photoaging, tends to accentuate the appearance of STLs.
In the repair of STLs, the correct placement of the long axis of an excision parallel to the STLs results in better scar cosmesis. Furthermore, flaps should be placed to allow the suture lines to fall in STLs. Although STLs may vary between individuals, some areas of the face have greater variability than others. Typically, the forehead, which has 1 major muscle group that pulls it vertically, has little individual variability; nearly everyone has horizontal STLs. In comparison, anatomic areas where multiple muscles act in different directions are likely to have greater variability.
In elderly patients, the direction of the relaxed STLs is generally obvious. In areas of ambiguity, excising the lesion as a circle and undermining it invariably pulls the surgical defect into an oval with the long axis corresponding to the relaxed STL.
Cosmetic Units and Subunits
Junction lines are fixed landmarks that separate the cosmetic units of the face.
Placing the suture lines on these boundaries (eg, eyebrow, nasolabial fold) optimizes scar formation. When a surgical wound is closed, repairing the wound in a cosmetic unit along a junction line is best. In larger defects that require a flap, the best results are achieved by using tissue from the same or adjacent cosmetic unit and by placing suture lines on the boundaries of those units. Subunits within cosmetic units are often subtle and individually variable. Paying attention to subtleties such as color, texture, sebaceous features, and hair characteristics help in identifying the changes between the subunits.
The scalp and forehead are individual cosmetic units that are separated by the hairline. In a bald individual, the top horizontal forehead crease serves as the junction line. Subunits of the forehead include the glabella, temples, and eyebrows.
The eyelids are a complex structure with multiple subunits that mimic the underlying orbicularis oculi muscle. The largest component of the eyelid is the orbital portion, which borders the eyebrow superiorly and the cheek inferiorly. Just below the eyebrow is the preseptal area and then the pretarsal portion where eyelashes insert. Additional components of the eyelid include the superior palpebral fold, the palpebral fissure, the medial limbus, and the medial canthus.
The cheek region is subdivided by the anterior prominence of the clenched masseter muscle. The masseter-parotid region lies posterior to this landmark and is posteriorly bound by the ear. The mandibular region lies anterior to the masseter and inferior to the lower lip. The malar subunit is around the zygoma anterior to the masseter muscle. This subunit is referred to as the anterior region.
The subdivisions of the external ear allow for good clinical descriptions of skin lesions in this location.
The nose1 has the most subdivisions on the face.
The horizontal root, which borders the glabella on the forehead, is positioned superiorly. The mid nose contains the dorsum medially and is flanked by the 2 lateral sidewalls. The dorsum is inferiorly bordered by the tip, which ends in the columella. The columella is the thin sliver of tissue that separates the nostrils on the underside of the nose. The tip is bordered by the ala nasi, or alae, on both sides, and the columella is flanked by the soft triangles, which also border the tip and the alae.
The lower part of the face is dominated by the subunits of the lip.
Below the nose in the moustache area are the cutaneous regions of the upper lip, which are separated from the cheek by the nasolabial fold. The middle depression below the nose, known as the philtrum, is an important anatomic subunit because even minimal displacement of this structure results in significant disfigurement. The lips constitute the vermilion subunit. The cutaneous lower lip, which borders the chin inferiorly and is bound by the nasolabial fold laterally, is below the vermillion.
Muscles of Facial Expression and the Superficial Musculoaponeurotic System
Muscles of facial expression
The muscles of facial expression are unique in a number of ways. Rather than inserting into bones or tendons, all of the muscles of facial expression originate from or insert into the skin. They are all derived from the second embryonic branchial arch and are innervated by the seventh cranial (facial) nerve. Different anatomic areas of the face have synergistic and antagonist groups of muscles that enable individuals to make varied facial expressions.
Muscles affecting the forehead and eyebrow include the frontalis muscle, which creates the horizontal wrinkles on the forehead and assists with eyebrow elevation, and the corrugators and procerus muscles, which are antagonistic muscles on the forehead. The orbicularis oculi muscles are a complex of muscles surrounding the eyes; these assist with closing the eye tightly. This muscle lies superficially in the eyelid skin and is encountered with even a shallow incision. The dominant muscle of the nose is the nasalis muscle, which consists of nasal and alar components. Its function is to compress and dilate the nares.
The mouth has the most extensive network of facial musculature and accounts for much of an individual's capability of facial expression. The orbicularis oris encircles the mouth and is the major component of the lips. The major functions of the orbicularis oris muscle are to pull the lips against the teeth, to draw the lips together, to pull the corners of the mouth together, and to pucker. This muscle is also extremely important for the phonation of sounds that rely on the lips, such as the pronunciation of the letters M, V, F, and P.
A group of 6 muscles, collectively known as the quadratus labii superioris muscle, controls the upper mouth. The 6 muscles are as follows:
- The zygomaticus major muscle starts from the posterolateral zygomatic bone and travels medially to insert on the upper portion of the orbicularis oris muscle. The zygomaticus major muscle helps in forming the lower nasolabial fold and is primarily responsible in smiling.
- The zygomaticus minor muscle arises just medially to the zygomaticus major and assists with its functions.
- The levator labii superioris muscle arises from the inferior portion of the maxilla and inserts on the upper lip, more medially than the zygomaticus muscles. The levator labii superioris muscle helps elevate the medial part of the upper lip and assists the zygomatic muscles with open smiling. The levator and zygomaticus muscles form the nasolabial fold.
- The levator anguli oris muscle is the most deeply positioned of the lip elevators and inserts on the upper corner of the mouth to assist with lip elevation.
- The risorius muscle arises over the parotid gland, inserts into the skin and mucosa of the lateral corner of the mouth, and assists with smiling. The risorius is not always present.
- The buccinator muscle is neither an elevator nor a depressor of the lip. It arises just posterior and medial to the last molar tooth and extends forward to become continuous with the orbicularis oris muscle. The buccinator muscle is the major component of the cheek musculature and prevents overdistension of the cheek (eg, in playing a wind instrument). This muscle assists the orbicularis oris muscle in whistling.
The depressors of the lip include the depressor anguli oris, the depressor labii inferioris, and the mentalis muscles. The marginal mandibular branch of the facial nerve innervates the depressors of the lip.
- The depressor anguli oris muscles arise from the lateral part of the mandible and travel superomedially to insert, with the orbicularis oris muscle, in the corners of the mouth. They function to depress and retract the corners of the mouth.
- The depressor labii inferioris muscles arise more medially on the mandible and travel superiorly to insert, with the orbicularis oris muscle, in the lower and medial part of the lip. Similar to the depressor anguli oris muscle, these muscles assist with the depression and retraction of the lower lip.
- The mentalis muscle, which is deep to both the depressor anguli oris and labii inferioris muscles, arises from the mandible and lower lateral incisor and courses inferiorly to insert on the skin covering the chin. The mentalis muscle elevates and wrinkles the chin and assists in protruding the lower lip.
Superficial musculoaponeurotic system
The facial musculature must work synergistically to allow for a wide range of facial expressions. The superficial musculoaponeurotic system (SMAS) is a discrete fibromuscular layer that envelops and interlinks the muscles to provide these synergies. The SMAS delineates the dissection planes for the extensive undermining necessary in facial rejuvenation procedures.
In addition, the SMAS serves as a useful marker in assessing the location of vital blood vessels and nerves. The superficial portion of the SMAS generally houses the axial blood vessels and sensory nerves, whereas the deeper levels contain the more vital motor nerves. The SMAS is generally located beneath the subcutaneous fat and superficial to the muscles. Superior to the zygoma, the SMAS links the temporalis, frontalis, occipitalis, and procerus muscles into a freely moveable continuous plane that connects with the subgaleal space. Inferiorly, the fascial anatomy is unclear; however, the SMAS interconnects the platysma, risorius, and depressor anguli oris muscles inferior to the zygoma. The muscles of the medial aspect of the face, including the orbicularis oculi, lip elevator, and nasal muscles, are not ensheathed by an interconnected SMAS.
Nerves
Sensory nerves
The trigeminal nerve, or cranial nerve (CN) V is primarily responsible for the sensory innervation of the face. The cervical, facial, glossopharyngeal, and vagus nerves have smaller contributions. The sensory nerves are typically located more superficially than the motor nerves, along the junction of the fat and the SMAS. Transection of the sensory nerves does not result in the serious morbidity that motor nerve damage causes, and the recovery of sensory function after such injury is typical.
The trigeminal nerve is divided into 3 branches: ophthalmic (CN V1), maxillary (CN V2), and mandibular (CN V3).
The V1 division provides sensation to the anterior part of the scalp, forehead, upper eyelid, and nasal bridge. Branches that arise around the superior orbital rim include the supraorbital, supratrochlear, infratrochlear, external nasal, and lacrimal branches. The V2 division supplies sensation to the lower eyelid, nasal sidewalls and columella, temple, and upper lip. Its major branch is the infraorbital nerve, which emerges from the infraorbital foramen with the infraorbital artery and vein. Other smaller branches include the zygomaticofacial and zygomaticotemporal nerves. The V3 division is the largest and most complicated of the divisions of CN V. It is the only division that carries motor fibers. The mandibular nerves provide sensation to the lower lip, chin, mandible, and preauricular areas.
The auriculotemporal, buccal, and mental nerves are the 3 major cutaneous branches of the mandibular nerve. The auriculotemporal nerve sends sensory fibers to the auricles, temples, and temporal parietal aspect of the scalp. In addition, it provides sensation to the external auditory canals, eardrums, and temporomandibular joints, and it carries some secretory fibers to the parotid glands. The buccal nerve is inaccessible for nerve blocks because of its deep location. It sends fibers to the cheek, mucosa, and gingiva. The mental nerve is the continuance of the inferior alveolar nerve, and it emerges from the mental foramen on the chin. It provides sensation to the chin, lower lip, mucosa, and gingiva of the lower lip. The motor component of the trigeminal nerve primarily innervates the muscles of mastication.
The cervical plexus lies deep to the sternocleidomastoid muscle. The plexus provides sensation to several important structures and is derived from C2 through C4. These nerves include the great auricular (C2, C3), lesser occipital (C2), greater occipital (C2), third occipital (C3), transverse cervical (C2, C3), and supraclavicular nerves. They send sensory fibers to the neck, posterior part of the ear, and postauricular scalp. The spinal accessory and cervical nerves emerge near the Erb point in the posterior triangle on the neck and are easily damaged during cutaneous surgery.
Lastly, sensory branches of the vagus, glossopharyngeal, and facial nerves innervate the skin of the external auditory canal, the concha, and the posterior sulcus. Awareness of the sensory branches of the face allows the use of nerve blocks, which provide effective anesthesia with minimal discomfort for the patient. Mental, infraorbital, and supraorbital blocks are easily achieved after the identification of their respective foramina, which lie in the midpupillary plane.
Motor nerves
CN VII, also known as the facial nerve, provides motor innervation to all the muscles of facial expression. CN VII also provides motor fibers to the digastric, stylohyoid, and stapedius muscles. In addition, sensory innervation to the anterior two thirds of the tongue, external auditory meatus, soft palate, and pharynx is mediated via the facial nerve. The motor portion of the facial nerve is divided into 5 major branches, but individual variation is common, with numerous smaller arborizations emanating from each major branch. The main facial nerve trunk emerges from the stylomastoid foramen, which is covered by the mastoid process, and along the posterior deep portion of the parotid gland. The main facial nerve trunk then divides into the temporal, zygomatic, buccal, mandibular, and cervical branches.
The temporal branch innervates the muscles of the upper part of the face including the upper orbicularis oculi, frontalis, and corrugator muscles. This branch is extremely susceptible to inadvertent injury because it travels superficially when it crosses the middle portion of the zygoma.
Transection of the temporal branch most prominently leads to unilateral frontalis dysfunction, which leaves the patient with ptosis and the inability to raise his or her eyebrows.
The zygomatic branch provides motor fibers to the lower orbicularis oculi, procerus, some lip elevator, and some nasal muscles.
The buccal branch often has numerous anastomotic connections with the zygomatic branch and sends fibers to similar muscles, in addition to the buccinator, orbicularis oris, depressor anguli oris, and risorius muscles. The buccal and zygomatic branches travel superficially over the buccal fat pad and just below the SMAS. This orientation makes them susceptible to injury during face-lift procedures. Transection of the nerves of the zygomatic and buccal branch leads to unpredictable defects, because muscular innervation in the mid face is variable.
In general, the marginal mandibular nerve does not have anastomotic connections. It innervates the orbicularis oris and lip depressor muscles. The anatomic course of the marginal mandibular nerve is unpredictable, but it should be considered in any excision near the angle of the mandible and the inferior margin of the parotid gland. Transection of the marginal mandibular nerve leads to extreme cosmetic and functional loss because the muscles of the mouth enable a significant amount of facial expression. The marginal mandibular branch of the facial nerve has a superficial course near the mandible and chin. This nerve usually lies anterior to the facial artery, which is palpable anterior to a clenched masseter muscle.
Transection of this nerve results in a droopy lip and subsequently drooling. Excisions on the lips can also lead to drooling, but not because of the transection of a motor nerve in this location.
The cervical branch is posterior and deep to the marginal mandibular nerve and innervates the platysma muscle. The cervical branch is of little importance to the cutaneous surgeon because its transection does not result in great functional or cosmetic loss.
The cutaneous surgeon must be aware of the delayed effects of local anesthetic on motor fibers. The unmyelinated sensory fibers lose conduction instantaneously, whereas the deeper myelinated motor fibers may lose their function only after a prolonged procedure with possibly greater anesthetic volume. Thus, the surgeon should not be alarmed by the delayed onset of a facial muscle paralysis. This effect on the motor nerves can last as long as 12 hours, and the patient should be appropriately counseled.
Blood Vessels
The external carotid artery provides most of the arterial blood supply to the face; the internal carotid artery makes a smaller contribution. The external carotid artery is the origin of the facial artery deep to the mandible near the pharynx. The facial artery courses around the jaw anterior to the masseter, where it is palpable, and continues superomedially to end as the angular artery near the medial canthus. Along its path, the facial artery serves as the origin to the inferior and superior labial arteries as well as smaller nasal branches. It provides the arterial blood supply to the lips and the middle of the face. At its terminal point, the facial artery connects with the ophthalmic artery, which provides important anastomoses with the internal carotid system.
Prior to its terminal differentiation, the external carotid artery results in the occipital and posterior auricular arteries, which supply the posterior part of the scalp and the postauricular areas. The terminal branches of the external carotid artery are the superficial temporal and internal maxillary arteries.
The superficial temporal artery arises in the parotid gland superficial to the branches of the facial nerve. The artery courses superiorly and results in the horizontal transverse facial artery 2 cm inferior to the zygoma; the resultant artery connects with the facial artery. As it continues superiorly, the superficial temporal artery also becomes more superficial and is palpable posterior to the temporal mandibular joint and anterior to the ear. The superficial temporal artery terminates in the parietal and frontal branches, which deliver blood to the scalp. Along its course, the superficial temporal artery provides blood to the lateral part of the face, the temple, the forehead, and the scalp. It also serves as the origin for smaller middle temporal and zygomatico-orbital arteries that supply some midfacial structures.
The internal maxillary is a deep artery that forms where the superficial temporal artery arises from the external carotid artery. Because of its deep location, the cutaneous surgeon rarely encounters the internal maxillary artery. Important branches of this artery include the infraorbital artery and the inferior alveolar artery, which continues through the mental foramen as the mental artery to provide blood to the chin.
The internal carotid artery supplies arterial blood to the eyelids, the upper and dorsal parts of the nose, the lower part of the forehead, and the scalp. The important major branch of the internal carotid artery is the ophthalmic artery. The ophthalmic artery has supraorbital, supratrochlear, infratrochlear, dorsal nasal, and external nasal branches that may form anastomoses with the external carotid system through the angular artery.
The venous network of the face parallels the arterial system. Unlike the arteries, the veins tend to be straighter and less tortuous. The facial vein parallels the facial artery and drains blood from the middle of the face into the internal jugular vein. The venous system of the medial aspect of the face (the dangerous triangle) involves the drainage of the upper lip and paranasal areas. In this area, the facial vein directly connects with the cavernous sinus, via the ophthalmic vein or indirectly connects with it, via the pterygoid plexus. The lateral part of the face and the scalp drain into the superficial temporal and retromandibular veins, which lead into the external jugular vein.
Lymphatics
The cutaneous surgeon often removes malignancies that can cause lymph node metastases. Knowledge of lymph flow is essential for an adequate clinical examination of the lymph nodes. Lymph flows from superficial areas to deep areas and then flows along 4 major tracts in an inferolateral direction to the collecting nodes in the neck and jaw. Great individual variability exists in the lymph flow; however, a general framework exists.
All the lymphatic fluid from the face eventually collects in a triangle of lymph nodes in the neck. The transverse cervical chain forms the inferior horizontal leg of the triangle, the spinal accessory chain forms the lateral leg, and the internal jugular chain forms the medial leg. The superior point of the triangle includes the superficial cervical and parotid nodes. The legs of the triangle are known as the deep lateral cervical nodes.
At the junction of the internal jugular and transverse cervical chains, the lymphatics enter the venous circulation at the jugulosubclavian junction. The spinal accessory chain travels along the spinal accessory nerve, making its removal more treacherous. This chain may be involved with early metastases from malignancies in the nasopharyngeal and thyroid areas. The transverse cervical chain is found along the transverse cervical vessels above the clavicle. The internal jugular chain is the major collection point for the head and neck, and it is divided into anterior and lateral divisions. By turning the patient's chin ipsilaterally and by rolling the relaxed sternocleidomastoid muscles between his or her fingers, the physician can clinically examine this group.
The postauricular node can be single or multiple, and it is located in the mastoid area attached to the insertion of the sternocleidomastoid muscle. Drainage from the ear can course anteriorly to the parotid nodes or inferiorly to the spinal accessory and internal jugular chains. Superficial and deep occipital nodes drain the posterior aspect of the scalp and the nuchal area. These nodes subsequently flow into the spinal accessory chain.
The parotid nodes have extraglandular and intraglandular components. The extraglandular nodes include the preauricular and infra-auricular subnodes and are located in the parotid fascia. These nodes function as a unit with the intraglandular nodes, which are deep in the gland. The parotid nodes drain into the submandibular chain or transverse cervical chain.
The facial nodes drain the mid face and are extremely variable between individuals. From superior to inferior, they are the infraorbital, malar, buccinator, and mandibular nodes. When present, these nodes are found in the subcutaneous layer above the muscles of the face. The facial nodes drain into the submandibular and submental chains.
The submandibular nodes are divided into 5 groups on the basis of their relationship to the facial vein and the submandibular gland. The preglandular nodes are below the platysma and anterior to the gland. The prevascular node is in the precarious position on the facial artery and touches the marginal mandibular nerve.
The postvascular nodes are also adjacent to the motor nerve. The existence of a retroglandular group is disputed. The submandibular gland surrounds a large group of intracapsular nodes. Many individuals have palpable nodes in the submandibular triangle. For clinical examination, the submandibular nodes can be palpated when the patient relaxes his or her neck muscles and moves his or her chin downward.
The submental nodes are above the mylohyoid and deep to the platysma in the submental triangle. The nodes drain the middle two thirds of the lower lip, the medial aspect of the cheek, and some facial nodes, and they can drain into the ipsilateral and contralateral nodes in the neck. Examination of the submental nodes is best accomplished by bimanually palpating the floor of the mouth and by pushing up under the patient's chin.
The superficial lateral cervical nodes receive drainage from the parotid, submandibular, and postauricular nodes. These cervical nodes are located on the superior external jugular vein, and some believe that they are part of the parotid infra-auricular nodes. The superficial lateral cervical nodes drain into the internal jugular chain.
Cutaneous Anatomy of the Neck
Muscles of the neck
The key cutaneous muscles of the neck are the platysma and sternocleidomastoid muscles. The platysma is covered by the SMAS, which is continuous with the lower muscles of the face, and it is also considered a muscle of facial expression. The platysma is an extremely thin muscle that is superficial in the neck. The sternocleidomastoid muscle extends from the medial clavicle to the postauricular area and divides the neck into posterior and anterior triangles.
Key components of the anterior triangle include the internal and external carotid arteries, the internal jugular vein, and the vagus and hypoglossal nerves. The important structure to consider to the posterior triangle is the spinal accessory nerve (CN XI), which innervates the sternocleidomastoid and trapezius muscles. Transection of the spinal accessory nerve results in a winged scapula and difficulty with arm abduction. The superficial cervical plexus is also found in the posterior triangle. The superficial cervical plexus has sensory, motor, and sympathetic functions.
A crucial anatomic landmark in the posterior triangle is the Erb point. The spinal accessory, great auricular, lesser occipital, and transverse cervical nerves all pass within 2 cm above or below this location. The Erb point can be located by drawing a line between the angle of the mandible and the mastoid process with the patient's head slightly turned. The Erb point lies at the junction of the posterior border of the sternocleidomastoid muscle and the point 6 cm inferior to the midpoint of the line drawn.
Blood vessels of the neck
The key blood vessels of the neck include the common and external carotid arteries and the jugular veins. The common carotid, internal jugular, and vagus nerves are found in the carotid sheath under the sternocleidomastoid and infrahyoid muscles before the carotid arteries bifurcate into their external and internal branches.
The external jugular vein forms below the parotid gland and travels inferiorly along the surface of the sternocleidomastoid muscle. The external jugular vein empties into the subclavian or internal jugular veins after it pierces through the superficial portion of the deep cervical fascia in the posterior triangle.
Skin tension lines
STLs typically lie in a transverse direction on the neck. The placement of excision lines in this orientation is essential because hypertrophic or reddened scars often result from misplaced excisions on the neck.
Anatomic Surgical Pearls
Free margins are located on the eyelids, helices of the ears, lips, and alar rim and columella. Unopposed tension caused by a surgical repair may distort these structures. Wound closure in these locations often require flap and/or graft placement to lessen the risk.
When designing flaps, borrow tissue from the same or adjacent cosmetic units to minimize anatomic distortion and maximize tissue match.
A reservoir of skin for flaps or primary closure can be found on the lower and posterior part of the cheek near the angle of the mandible. In older persons, this area is the jowl. Other areas with redundant skin include the preauricular aspect of the cheek, the temple, and the neck.
Place the suture lines along STLs and on the boundaries of the cosmetic units whenever possible.
Preoperatively identify the vital structures that might be damaged in the operative field, and stay vigilant to avoid them. Examples of vital structures include the temporal nerve in the upper part of the cheek and temple, the marginal mandibular nerve on the jaw line, and CN XI at the Erb point.
Identify sensory innervation to structures in the operative field, and perform a nerve block wherever possible to minimize the patient's discomfort and distortion of the operative field by using large amounts of lidocaine. Examples of sensory innervations include the mental nerve on the chin and the supraorbital and supratrochlear nerves in large lesions on the forehead.
When working in deeper planes, attempt to identify the SMAS, which can help in locating and avoiding vital vessels and nerves.
Multimedia
 | Media file 1: Skin tension lines. Illustrated by Charles Norman. |
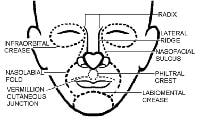 | Media file 2: Cosmetic subunits. Illustrated by Charles Norman. |
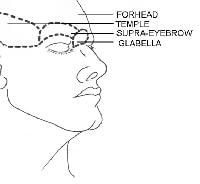 | Media file 3: Forehead subunits. Illustrated by Charles Norman. |
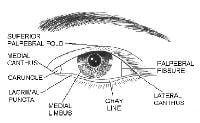 | Media file 4: Eyelid subunits. Illustrated by Charles Norman. |
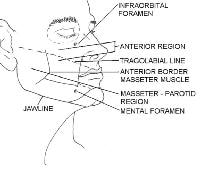 | Media file 5: Subunits of the anterior region. Illustrated by Charles Norman. |
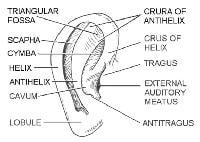 | Media file 6: Subunits of the ear. Illustrated by Charles Norman. |
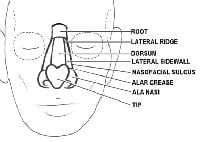 | Media file 7: Subunits of the nose. Illustrated by Charles Norman. |
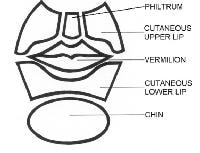 | Media file 8: Subunits of the lower part of the face. Illustrated by Charles Norman. |
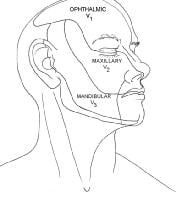 | Media file 9: Distribution of cranial nerve V. Illustrated by Charles Norman. |
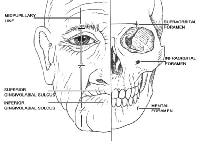 | Media file 10: Foramina for nerve blocks. Illustrated by Charles Norman. |
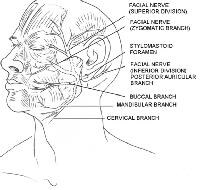 | Media file 11: Branches of the facial nerve. Illustrated by Charles Norman. |
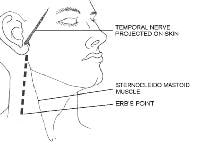 | Media file 12: Course of the temporal nerve and location of the Erb point. Illustrated by Charles Norman. |
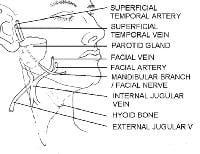 | Media file 13: Course of the marginal mandibular nerve. Illustrated by Charles Norman. |
Keywords
skin tension lines, STLs, cosmetic units, muscles of facial expression, face muscles, facial muscles, superficial musculoaponeurotic system, SMAS, sensory nerves, motor nerves, blood vessels, lymphatics, anatomy of the neck, neck muscles, anatomic surgical pearls





0 comments:
Post a Comment