Thoracic Aortic Aneurysm
Thoracic Aortic Aneurysm;
Definition
Anatomically and radiologically, an aneurysm is defined as a dilatation at least 50% above the normal diameter of the artery. In the thoracic aorta, a diameter of 3 cm or greater is generally considered aneurysmal, although the average size of surgically corrected aneurysms is over 5 cm. Thoracic aortic aneurysm (TAA) can involve the aortic root, ascending aorta, arch, descending aorta, or a combination of these locations. The combination of aortic root dilatation and ascending aneurysm is termed “annuloaortic ectasia.”Aortic dissections are frequently superimposed on noninflammatory thoracic aortic aneurysm (TAA); these are often designated “dissecting aneurysms.” However, aortic dissections may occur with medial degeneration in the absence of pre-existing aneurysm (“aortic dissection”). Pseudoaneurysm denotes a ruptured aortic wall with healing of the extravasated blood and formation of the aneurysm wall by fibrous tissue.
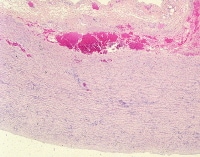
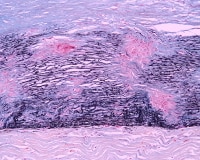
A 29-year-old man, sudden death. Low magnification of aortic wall with dissection plane between the media and the adventitia (right to left of the photograph). The media shows mild mucoid deposition and degeneration. There was no history of a genetic syndrome.
Epidemiology
Aortic aneurysms are a leading cause of the death in the United States. With improvements in screening and imaging techniques, the incidence of thoracic aortic aneurysm (TAA) has been increasing steadily in the last decades. Overall, the estimated incidence of thoracic aortic aneurysm (TAA) is 6 cases per 100,000 person-years. Autopsy series have estimated its prevalence of 3-4% in patients over 65 years of age.
The cause of thoracic aortic aneurysm (TAA) greatly affects the age at presentation. Patients with inherited disorders have thoracic aortic aneurysm (TAA) at an early age, presenting in childhood or adolescence. Patients with idiopathic noninflammatory aneurysms are typically adults and present with symptoms of aneurysms later than those patients with identified connective tissue disorders. Patients with aortitis and aneurysms present at middle age and older, including advanced ages, especially in the case of giant cell aortitis. An approximately 2:1 male predilection for noninflammatory thoracic aortic aneurysm (TAA) exists;1,2 inflammatory thoracic aortic aneurysm (TAA) is slightly more common in women.
The cause of thoracic aortic aneurysm (TAA) greatly affects the age at presentation. Patients with inherited disorders have thoracic aortic aneurysm (TAA) at an early age, presenting in childhood or adolescence. Patients with idiopathic noninflammatory aneurysms are typically adults and present with symptoms of aneurysms later than those patients with identified connective tissue disorders. Patients with aortitis and aneurysms present at middle age and older, including advanced ages, especially in the case of giant cell aortitis. An approximately 2:1 male predilection for noninflammatory thoracic aortic aneurysm (TAA) exists;1,2 inflammatory thoracic aortic aneurysm (TAA) is slightly more common in women.
Etiology
Causes of thoracic aortic aneurysm (TAA) include inherited syndromes, atherosclerosis, noninfectious aortitis, and infections; however, a large number have no known cause. Idiopathic noninflammatory aneurysms are associated with congenital conditions (bicuspid aortic valve) and acquired conditions (hypertension). Pathologically, noninflammatory aneurysms demonstrate degrees of cystic medial degeneration, depending on etiology or association. The inherited syndromes causing thoracic aortic aneurysm (TAA) include Marfan syndrome, Loeys-Dietz syndrome, and Ehlers-Danlos syndrome.
Aneurysmal dilatation of the thoracic aorta can occur by various mechanisms. Most commonly, the pathogenesis of the aneurysms is due to noninflammatory medial degeneration of the elastic aortic wall, but inflammatory destruction, secondary to syphilis, bacterial infection, noninfectious aortitis, or atherosclerotic can result in thoracic aortic aneurysm (TAA). Pseudoaneurysms may result from aortic tears, typically due to blunt chest trauma, with healing of the extravasated blood and formation of fibrous tissue wall.
The etiology of thoracic aortic aneurysm (TAA) depends on the site in the aorta. Most surgically resected thoracic aortic aneurysms (TAA) involve the ascending aorta. In a series of 513 ascending thoracic aortic aneurysm (TAA) at the Mayo Clinic, 13% of patients had inherited connective tissue disease, mostly Marfan syndrome;3 25% had bicuspid aortic valve with noninflammatory thoracic aortic aneurysm (TAA); 11% had aortitis; and the remaining 51% had idiopathic noninflammatory aneurysms, of whom approximately 60% were hypertensive.
Atherosclerosis accounts for only 1% of ascending thoracic aortic aneurysm (TAA);3 however, 90% of descending thoracic aortic aneurysm (TAA) are atherosclerotic,4 the remaining 10% comprising chronic dissections. Descending thoracic aortic aneurysm (TAA) are less frequently resected than ascending thoracic aortic aneurysm (TAA), as they are frequently treated medically, especially chronic dissections.5
Medial degeneration is the histologic substrate for most dissecting aneurysms and annuloaortic ectasia. Aortitis is divided clinically and pathologically in 2 major types, Takayasu arteritis and giant cell arteritis (GCA).6 The remaining etiologies account for less than 1-5% of surgical resections. Syphilitic aneurysms result in marked aortic root dilatation with ascending aneurysms but are extremely rare in developed countries.6 Infectious bacterial aneurysms, still often termed “mycotic aneurysms” after the designation given by Osler in the 1800s,7 are frequently seen in patients with bacteremia due to infectious endocarditis. Most pseudoaneurysms are the result of trauma or ruptured atherosclerotic ulcers and may occur in any portion of the aorta, but typically occur in the descending thoracic aorta.8
Marfan syndrome (MFS) is an autosomal dominant disorder characterized by abnormalities of the eyes, skeleton, and cardiovascular system. MFS is an autosomal dominant disease, with one quarter of patients not having a family history and getting the disease from new mutations. Aortic root dilatation, aortic dissections, mitral valve prolapse, and other miscellaneous cardiovascular manifestations are seen in MFS. Patients with MFS have medial degeneration of the aorta, also referred to as cystic medial necrosis. The histologic medial degeneration tends to be prominent in patients with this syndrome, although not specific to the disease.
Loeys-Dietz syndrome (LDS) is an autosomal dominant connective tissue disorder that is a rare cause of thoracic aortic aneurysm (TAA). It results from genetic mutations in the transforming growth factor beta receptors 1 and 2 (TGFBR1 and TGFBR2). The syndrome is characterized phenotypically by hypertelorism, bifid uvula, and/or cleft palate, and arterial tortuosity with aneurysms and dissections. LDS has a much more rapid clinical course than Marfan syndrome (MFS); thus, those diagnosed with LDS are currently being recommended for prophylactic aortic root replacement at younger ages and with smaller aortic dimensions. Histologically, diffuse medial degeneration, which may be subtle, exists.9
Patients with Ehlers-Danlos syndrome type IV may also have thoracic aortic aneurysms; however, the typical complication is rupture in normal caliber artery. Coronary artery dissections, aortic rupture, iliac and femoral rupture, and coronary and other muscular arterial aneurysms are among the different complications seen in these patients.
Although most non-Marfan thoracic aortic aneurysms (TAA) are sporadic, familial aggregation studies have suggested a higher prevalence in first-degree relatives.10,11 In a large study of 470 patients with thoracic aortic aneurysms (TAA) and no history of Marfan syndrome, family history studies found an inherited pattern in 21.5% of patients. These patients were significantly younger than patients without a family history, but older than full-blown Marfan syndrome. In over 75% of families with multiple affected members, the disease is inherited in an autosomal-dominant manner. Interestingly, an increased risk of abdominal aortic aneurysm, cerebral, and other aneurysms exists.12 Various loci have been recently associated with familial thoracic aortic aneurysm (TAA), which includeTAAD1, FAA1, FBN1, and others.
A significant clinical association with thoracic aortic aneurysm (TAA) with or without dissection is congenitally bicuspid aortic valve (BAV). BAV is a common congenital defect affecting approximately 1.3% of the general population, but 14% of patients with proximal aortic dissections.13 The development defect underlying the association between aortic root dilatation and dissection is unknown, but both conditions have a hereditary component. It is currently accepted that the aneurysms are not due to flow-related disturbances secondary to valvar insufficiency or stenosis; for this reason, wrapping of the aorta to prevent progressive dilatation after valve repair is often advocated.14
Patients with bicuspid aortic valve and thoracic aortic aneurysm (TAA) present at a mean age of 56 +/- 13 years); one-half have aortic valve stenosis, and the other have valve insufficiency, with or without stenosis; only a small number have normal valve function.12 Among patients with thoracic aortic aneurysm (TAA) and aortic insufficiency, the two-thirds of the valve insufficiency can be treated with ascending aortic aneurysm repair, and the remainder requires valve replacement.1
Infections are a rare cause of thoracic aortic aneurysm (TAA). In developed countries, syphilitic aortitis is vanishingly rare, accounting for 0-1% in various series.6 Bacterial (“myocytic”) aneurysms are a rare cause of ascending thoracic aortic aneurysm (TAA) and descending thoracic aortic aneurysm (TAA). In one series of 734 patients with aortic aneurysms, only 2.3% were caused by bacterial infection, and most occurred in the abdominal aorta. The most common pathogens were Salmonella and Staphylococcus species.7 Many patients have a prior history of endocarditis.
Rare causes of thoracic aortic aneurysm (TAA) include posttraumatic pseudoaneurysms, most frequently seen in the proximal descending thoracic aorta at the site of the ligamentum arteriosum, where blunt chest trauma results in separation of the aortic wall.8 Congenital thoracic aortic aneurysm (TAA) may occur in association with aberrant right subclavian artery with diverticulum of Kommerell.15
The etiology of the aneurysm may affect the incidence of dissections. Atherosclerosis, when advanced, typically results in medial and adventitial fibrosis, which hampers the development of dissections. In some cases, an atherosclerotic plaque may ulcerate and result in limited dissection, so-called penetrating atherosclerotic ulcer.
These lesions are typically not aneurysmal but show imaging characteristics of intramural hematoma and usually occur in the descending thoracic aorta. Dissections are common in Marfan syndrome, idiopathic thoracic aortic aneurysm (TAA), and thoracic aortic aneurysm (TAA) associated with bicuspid aortic valve, because the medial degeneration is devoid of significant scarring and results in laminar weakness of the wall. Because rare examples of thoracic aortic aneurysm (TAA) with dissection lack an intimal tear, it is believed that the initiation of the dissection may involve leaking or rupture vasa vasorum, which are present predominantly in the proximal aorta. Inflammatory aortitides are associated with aneurysm, but the significant adventitial fibrosis that accompanies Takayasu aortitis inhibits dissections, despite the medial inflammation, whereas the aortitis of giant cell aortitis is more frequently associated with aneurysms, because fibrosis is less prominent.
Aneurysmal dilatation of the thoracic aorta can occur by various mechanisms. Most commonly, the pathogenesis of the aneurysms is due to noninflammatory medial degeneration of the elastic aortic wall, but inflammatory destruction, secondary to syphilis, bacterial infection, noninfectious aortitis, or atherosclerotic can result in thoracic aortic aneurysm (TAA). Pseudoaneurysms may result from aortic tears, typically due to blunt chest trauma, with healing of the extravasated blood and formation of fibrous tissue wall.
The etiology of thoracic aortic aneurysm (TAA) depends on the site in the aorta. Most surgically resected thoracic aortic aneurysms (TAA) involve the ascending aorta. In a series of 513 ascending thoracic aortic aneurysm (TAA) at the Mayo Clinic, 13% of patients had inherited connective tissue disease, mostly Marfan syndrome;3 25% had bicuspid aortic valve with noninflammatory thoracic aortic aneurysm (TAA); 11% had aortitis; and the remaining 51% had idiopathic noninflammatory aneurysms, of whom approximately 60% were hypertensive.
Atherosclerosis accounts for only 1% of ascending thoracic aortic aneurysm (TAA);3 however, 90% of descending thoracic aortic aneurysm (TAA) are atherosclerotic,4 the remaining 10% comprising chronic dissections. Descending thoracic aortic aneurysm (TAA) are less frequently resected than ascending thoracic aortic aneurysm (TAA), as they are frequently treated medically, especially chronic dissections.5
Medial degeneration is the histologic substrate for most dissecting aneurysms and annuloaortic ectasia. Aortitis is divided clinically and pathologically in 2 major types, Takayasu arteritis and giant cell arteritis (GCA).6 The remaining etiologies account for less than 1-5% of surgical resections. Syphilitic aneurysms result in marked aortic root dilatation with ascending aneurysms but are extremely rare in developed countries.6 Infectious bacterial aneurysms, still often termed “mycotic aneurysms” after the designation given by Osler in the 1800s,7 are frequently seen in patients with bacteremia due to infectious endocarditis. Most pseudoaneurysms are the result of trauma or ruptured atherosclerotic ulcers and may occur in any portion of the aorta, but typically occur in the descending thoracic aorta.8
Marfan syndrome (MFS) is an autosomal dominant disorder characterized by abnormalities of the eyes, skeleton, and cardiovascular system. MFS is an autosomal dominant disease, with one quarter of patients not having a family history and getting the disease from new mutations. Aortic root dilatation, aortic dissections, mitral valve prolapse, and other miscellaneous cardiovascular manifestations are seen in MFS. Patients with MFS have medial degeneration of the aorta, also referred to as cystic medial necrosis. The histologic medial degeneration tends to be prominent in patients with this syndrome, although not specific to the disease.
Loeys-Dietz syndrome (LDS) is an autosomal dominant connective tissue disorder that is a rare cause of thoracic aortic aneurysm (TAA). It results from genetic mutations in the transforming growth factor beta receptors 1 and 2 (TGFBR1 and TGFBR2). The syndrome is characterized phenotypically by hypertelorism, bifid uvula, and/or cleft palate, and arterial tortuosity with aneurysms and dissections. LDS has a much more rapid clinical course than Marfan syndrome (MFS); thus, those diagnosed with LDS are currently being recommended for prophylactic aortic root replacement at younger ages and with smaller aortic dimensions. Histologically, diffuse medial degeneration, which may be subtle, exists.9
Patients with Ehlers-Danlos syndrome type IV may also have thoracic aortic aneurysms; however, the typical complication is rupture in normal caliber artery. Coronary artery dissections, aortic rupture, iliac and femoral rupture, and coronary and other muscular arterial aneurysms are among the different complications seen in these patients.
Although most non-Marfan thoracic aortic aneurysms (TAA) are sporadic, familial aggregation studies have suggested a higher prevalence in first-degree relatives.10,11 In a large study of 470 patients with thoracic aortic aneurysms (TAA) and no history of Marfan syndrome, family history studies found an inherited pattern in 21.5% of patients. These patients were significantly younger than patients without a family history, but older than full-blown Marfan syndrome. In over 75% of families with multiple affected members, the disease is inherited in an autosomal-dominant manner. Interestingly, an increased risk of abdominal aortic aneurysm, cerebral, and other aneurysms exists.12 Various loci have been recently associated with familial thoracic aortic aneurysm (TAA), which includeTAAD1, FAA1, FBN1, and others.
A significant clinical association with thoracic aortic aneurysm (TAA) with or without dissection is congenitally bicuspid aortic valve (BAV). BAV is a common congenital defect affecting approximately 1.3% of the general population, but 14% of patients with proximal aortic dissections.13 The development defect underlying the association between aortic root dilatation and dissection is unknown, but both conditions have a hereditary component. It is currently accepted that the aneurysms are not due to flow-related disturbances secondary to valvar insufficiency or stenosis; for this reason, wrapping of the aorta to prevent progressive dilatation after valve repair is often advocated.14
Patients with bicuspid aortic valve and thoracic aortic aneurysm (TAA) present at a mean age of 56 +/- 13 years); one-half have aortic valve stenosis, and the other have valve insufficiency, with or without stenosis; only a small number have normal valve function.12 Among patients with thoracic aortic aneurysm (TAA) and aortic insufficiency, the two-thirds of the valve insufficiency can be treated with ascending aortic aneurysm repair, and the remainder requires valve replacement.1
Infections are a rare cause of thoracic aortic aneurysm (TAA). In developed countries, syphilitic aortitis is vanishingly rare, accounting for 0-1% in various series.6 Bacterial (“myocytic”) aneurysms are a rare cause of ascending thoracic aortic aneurysm (TAA) and descending thoracic aortic aneurysm (TAA). In one series of 734 patients with aortic aneurysms, only 2.3% were caused by bacterial infection, and most occurred in the abdominal aorta. The most common pathogens were Salmonella and Staphylococcus species.7 Many patients have a prior history of endocarditis.
Rare causes of thoracic aortic aneurysm (TAA) include posttraumatic pseudoaneurysms, most frequently seen in the proximal descending thoracic aorta at the site of the ligamentum arteriosum, where blunt chest trauma results in separation of the aortic wall.8 Congenital thoracic aortic aneurysm (TAA) may occur in association with aberrant right subclavian artery with diverticulum of Kommerell.15
The etiology of the aneurysm may affect the incidence of dissections. Atherosclerosis, when advanced, typically results in medial and adventitial fibrosis, which hampers the development of dissections. In some cases, an atherosclerotic plaque may ulcerate and result in limited dissection, so-called penetrating atherosclerotic ulcer.
These lesions are typically not aneurysmal but show imaging characteristics of intramural hematoma and usually occur in the descending thoracic aorta. Dissections are common in Marfan syndrome, idiopathic thoracic aortic aneurysm (TAA), and thoracic aortic aneurysm (TAA) associated with bicuspid aortic valve, because the medial degeneration is devoid of significant scarring and results in laminar weakness of the wall. Because rare examples of thoracic aortic aneurysm (TAA) with dissection lack an intimal tear, it is believed that the initiation of the dissection may involve leaking or rupture vasa vasorum, which are present predominantly in the proximal aorta. Inflammatory aortitides are associated with aneurysm, but the significant adventitial fibrosis that accompanies Takayasu aortitis inhibits dissections, despite the medial inflammation, whereas the aortitis of giant cell aortitis is more frequently associated with aneurysms, because fibrosis is less prominent.
Location
The location of thoracic aortic aneurysm (TAA) varies by etiology and is of critical importance in approaches to surgical repair. The sites of involvement include the aortic root (including the sinuses of Valsalva and fibrous annulus), the ascending aorta distal to the sinotubular junction, the transverse arch, and the distal thoracic aorta.
Ascending aortic aneurysms have several anatomic surgical subsets. Aortic root disease with or without ascending aortic involvement (annuloaortic ectasia) generally results in aortic insufficiency and requires valve replacement with valved ascending aortic graft (Bentall procedure). Aortic root dilatation is best determined by intraoperative transesophageal ultrasound.
Recently, valve sparing aortic root repair with root reconstruction with or without valve reimplantation has been developed.1 Ascending aortic aneurysms not involving the root may cause aortic insufficiency due to dilatation of the sinotubular junction, but aortic valve insufficiency is generally corrected by aneurysm repair only and valve replacement is not necessary. Ascending aneurysms may extend into the aortic arch, requiring partial or complete arch replacement; these aneurysms are often inflammatory or atherosclerotic. Aneurysms of the distal arch and descending aorta are typically atherosclerotic. The other common types of aneurysm involving the descending thoracic aorta are healed dissecting aneurysms, infectious (“mycotic”) aneurysms, and traumatic pseudoaneurysms.
Noninflammatory aneurysms caused by Marfan syndrome almost always involved the aortic root, necessitating valve replacement or valve-sparing root repair. Noninflammatory aneurysms in older patients often spare the aortic valve and root. Syphilitic aortitis, as well as noninfectious aortitis, typically involves the aortic root, which requires valve replacement or root repair in over 50% of patients.16,17
The location of the aneurysm also affects the prevalence of subtypes. Atherosclerotic lesions are most frequent in the descending aorta and the aortic arch. Aneurysms associated with medial degeneration are almost exclusively in the ascending segment, and dissecting aneurysms may be present either in the proximal or descending portion. Patients with aortitis tend to present with involvement of the ascending aorta. Infectious cases (mycotic mainly) are more frequent in the descending aorta.
Ascending aortic aneurysms have several anatomic surgical subsets. Aortic root disease with or without ascending aortic involvement (annuloaortic ectasia) generally results in aortic insufficiency and requires valve replacement with valved ascending aortic graft (Bentall procedure). Aortic root dilatation is best determined by intraoperative transesophageal ultrasound.
Recently, valve sparing aortic root repair with root reconstruction with or without valve reimplantation has been developed.1 Ascending aortic aneurysms not involving the root may cause aortic insufficiency due to dilatation of the sinotubular junction, but aortic valve insufficiency is generally corrected by aneurysm repair only and valve replacement is not necessary. Ascending aneurysms may extend into the aortic arch, requiring partial or complete arch replacement; these aneurysms are often inflammatory or atherosclerotic. Aneurysms of the distal arch and descending aorta are typically atherosclerotic. The other common types of aneurysm involving the descending thoracic aorta are healed dissecting aneurysms, infectious (“mycotic”) aneurysms, and traumatic pseudoaneurysms.
Noninflammatory aneurysms caused by Marfan syndrome almost always involved the aortic root, necessitating valve replacement or valve-sparing root repair. Noninflammatory aneurysms in older patients often spare the aortic valve and root. Syphilitic aortitis, as well as noninfectious aortitis, typically involves the aortic root, which requires valve replacement or root repair in over 50% of patients.16,17
The location of the aneurysm also affects the prevalence of subtypes. Atherosclerotic lesions are most frequent in the descending aorta and the aortic arch. Aneurysms associated with medial degeneration are almost exclusively in the ascending segment, and dissecting aneurysms may be present either in the proximal or descending portion. Patients with aortitis tend to present with involvement of the ascending aorta. Infectious cases (mycotic mainly) are more frequent in the descending aorta.
Clinical Features and Imaging
A large percentage of patients with thoracic aortic aneurysm (TAA) are asymptomatic. Thoracic aneurysms are usually found incidentally after imaging studies. Symptoms develop in the setting of aortic insufficiency (aneurysms involving the aortic root or ascending aorta), dissection, or rupture. Rupture may occur in the thinned aneurysm wall or as rupture of the false lumen of a prior dissection. Symptoms from rupture result from pain, hemopericardium (ascending aortic aneurysms), or hemothorax (descending aneurysms). Dissections may cause symptoms by rupture of the false lumen, or extension of the dissection into arch vessels, causing cerebral ischemia, or coronary vessels, and causing myocardial ischemia. The growth of aneurysm may be indolent, and debate exists as to the appropriate timing of surgical intervention, with suggestions as early as 3 cm to as late as 6 cm.
Symptomatic patients may experience symptoms of aortic insufficiency and heart failure, or pain that may be epicardial with radiation to the neck and jaw. Back pain, between the scapulae, is more likely to happen in patients with dissection of the descending aorta. When ruptured, patients with thoracic aortic aneurysm (TAA) experience about the greatest pain ever felt, and medical attention should be sought immediately, as the mortality rates increase rapidly by the hour.
Symptomatic patients may experience symptoms of aortic insufficiency and heart failure, or pain that may be epicardial with radiation to the neck and jaw. Back pain, between the scapulae, is more likely to happen in patients with dissection of the descending aorta. When ruptured, patients with thoracic aortic aneurysm (TAA) experience about the greatest pain ever felt, and medical attention should be sought immediately, as the mortality rates increase rapidly by the hour.
Gross Findings
Uncomplicated thoracic aortic aneurysms can be divided grossly into saccular and fusiform. Fusiform aneurysms are most common, and affect the entire circumference of the aorta and have tapered borders. Among the types of thoracic aortic aneurysm (TAA), only infectious (mycotic) aneurysms and posttraumatic pseudoaneurysms are typically saccular, both of which have a propensity for the distal thoracic aorta. Only rarely are aneurysms secondary to medial weakness due to medial degeneration saccular.
At autopsy, the gross appearance of thoracic aortic aneurysm (TAA) depends on the type. Proximal thoracic aortic aneurysms (TAA) demonstrate diffuse ectasia of the ascending aorta. Aneurysms of the proximal portion of the aorta may stretch the aortic ring, resulting in aortic insufficiency (annuloaortic ectasia). Involvement of the aortic root is typical of Marfan syndrome, syphilitic aneurysms, and a significant proportion of noninfectious aortitis. Syphilitic aneurysms tend to demonstrate massive aneurysm formation, and marked thinning of the aortic wall. In noninflammatory aneurysms, the arch is generally spared, but aortic aneurysms and atherosclerotic aneurysms frequently extend to the arch vessels.16
Distal thoracic aneurysms are typically atherosclerotic, and demonstrate diffuse ectasia of the lumen, with frequent extension across the diaphragm into the abdominal aorta (thoraco-abdominal aortic aneurysm). Infectious (mycotic) aneurysms may be saccular, and typically erode into adjacent structures with adhesions and tissue edema.
The adventitial appearance of thoracic aortic aneurysm (TAA) is generally unremarkable, unless true or false lumen is ruptured, resulting in soft tissue hemorrhage, or if, in the case of infectious aneurysm, adhesions and edema exist.
The intimal surface of an aneurysm may be normal, as in the case of noninflammatory aneurysm; may demonstrate wrinkled appearance of the intima of a healed dissection; may demonstrate “tree-barking” of an aortic or syphilitic aneurysm; or may demonstrate atherosclerotic plaques, in the case of atherosclerotic aneurysm. Superimposed atherosclerotic change may be found in aneurysms of Takayasu aortitis. One form of aneurysm or the ascending aorta is the so-called “egg-shell” aorta that occurs in cases of diffuse intimal calcification of atherosclerotic intima.
Dissecting aortic aneurysms represent one of the most dramatic specimens in gross pathology. The aneurysm involves the root in most cases of Marfan syndrome, but typically spares the root in patients with bicuspid aortic valve or idiopathic aneurysms. Aortic dissections have been studied extensively for centuries with uncountable descriptions in the medical and lay literature. The most common used classification is the one by DeBakey and colleagues from 1965.18 Three major types are described as follows:
At autopsy, the gross appearance of thoracic aortic aneurysm (TAA) depends on the type. Proximal thoracic aortic aneurysms (TAA) demonstrate diffuse ectasia of the ascending aorta. Aneurysms of the proximal portion of the aorta may stretch the aortic ring, resulting in aortic insufficiency (annuloaortic ectasia). Involvement of the aortic root is typical of Marfan syndrome, syphilitic aneurysms, and a significant proportion of noninfectious aortitis. Syphilitic aneurysms tend to demonstrate massive aneurysm formation, and marked thinning of the aortic wall. In noninflammatory aneurysms, the arch is generally spared, but aortic aneurysms and atherosclerotic aneurysms frequently extend to the arch vessels.16
Distal thoracic aneurysms are typically atherosclerotic, and demonstrate diffuse ectasia of the lumen, with frequent extension across the diaphragm into the abdominal aorta (thoraco-abdominal aortic aneurysm). Infectious (mycotic) aneurysms may be saccular, and typically erode into adjacent structures with adhesions and tissue edema.
The adventitial appearance of thoracic aortic aneurysm (TAA) is generally unremarkable, unless true or false lumen is ruptured, resulting in soft tissue hemorrhage, or if, in the case of infectious aneurysm, adhesions and edema exist.
The intimal surface of an aneurysm may be normal, as in the case of noninflammatory aneurysm; may demonstrate wrinkled appearance of the intima of a healed dissection; may demonstrate “tree-barking” of an aortic or syphilitic aneurysm; or may demonstrate atherosclerotic plaques, in the case of atherosclerotic aneurysm. Superimposed atherosclerotic change may be found in aneurysms of Takayasu aortitis. One form of aneurysm or the ascending aorta is the so-called “egg-shell” aorta that occurs in cases of diffuse intimal calcification of atherosclerotic intima.
Dissecting aortic aneurysms represent one of the most dramatic specimens in gross pathology. The aneurysm involves the root in most cases of Marfan syndrome, but typically spares the root in patients with bicuspid aortic valve or idiopathic aneurysms. Aortic dissections have been studied extensively for centuries with uncountable descriptions in the medical and lay literature. The most common used classification is the one by DeBakey and colleagues from 1965.18 Three major types are described as follows:
- Dissection involving both the ascending and descending aorta (Type I)
- Dissection only in the ascending aorta (Type II)
- Dissection involving only the descending aorta (Type III)
The outer wall of the false lumen is usually thinner than the inner dissected wall, thus rupture to adjacent structures (commonly causing hemopericardium, left pleural hemothorax, or extension of the blood into the mediastinum) is frequent. The distal portion of the false lumen will demonstrate a second communication with the true lumen, in the form of a re-entry tear. The intimal tears associated with aortic dissections heal over time, in cases of prolonged survival, and have a white fibrous surface.
Heart of a 43-year-old male sudden death case. External view of proximal aorta showing dilatation and transmural tear, after removal of blood clots from hemopericardium.
Coronal section with concentric left ventricular hypertrophy (left ventricular free wall=18mm). A proximal aneurysm of the aorta is seen (5 x 4 cm) with focal rupture and hemopericardium (not shown). The aortic valve (not shown) revealed minimal root dilatation. Histologic sections showed marked medial degeneration.
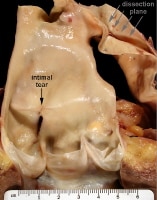
A 34-year old with no known medical history. He had vague complaints of abdominal pain and expired in emergency department prior to any medical care. The intimal tear measures 5mm and is just distal to the sinotubular junction. The dissection extends from aortic root through arch and into descending aorta, terminating 9cm proximal to the superior mesenteric artery ostium. There was no involvement of branch vessels. Note dissection place (multiple arrows).
Chronic aortic dissection in a 49-year-old man with history of hypertension. The dissection with proximal intimal tear at level of isthmus and double barrel lumen extending to abdominal aorta with re-entry tear above renal arteries. The false lumen contains organized thrombus and atheromatous plaque. The distal abdominal aorta (not shown) shows severe atherosclerosis with multiple ulcerated plaques; histologic sections of the dissection show no evidence of cystic medial necrosis.
A 36-year-old female patient; sudden cardiac death of cardiac tamponade from ruptured aortic aneurysm and hemopericardium. A fusiform aneurysm is seen just distal to the aortic valve (not shown). The patient was status post replacement of aortic valve for congenital bicuspid aortic valve.
A 41-year-old man presenting with back pain, died suddenly. Gross photograph showing circumferential hematoma dissecting the aortic wall proximally. There is only mild fusiform aneurysmal dilatation. The large longitudinal tear is located about 5 cm from the sinotubular junction.
A 68-year-old woman with fusiform dilatation of the ascending aorta and transverse intimal tear. Aortic valve is at left of the photograph. The dissection plane direction run proximally to dissect the left main coronary artery.
Microscopic Findings
Noninflammatory thoracic aortic aneurysm
The histopathologic hallmark of noninflammatory thoracic aortic aneurysm (TAA) is cystic medial degeneration, or the pooling of proteoglycans (mucoid material) and pseudocysts formation in the media, accompanied by extensive loss of elastic lamellae. These changes result in the medial weakening that progresses to aneurysm, dissection, or both. A related histologic finding is so-called “medionecrosis” a finding also seen in aging aortas and in patients with hypertension. Medionecrosis, or laminar medial necrosis, is defined as coagulative necrosis of medial smooth muscle cells, resulting in loss of nuclei and collapse of the elastic lamellae,3 a finding that is not specific for any specific etiology for thoracic aortic aneurysm (TAA).
Aneurysms associated with uni- and bicuspid aortic valve disease usually show focal loss of elastic laminae and some associated intimal fibrosis, which is usually mild. MFS patients usually have severe elastic fiber degeneration of the aortic media, which can be prominent at and around the sites of gross tears. If a healing process, such as remote tear, is present, intimal thickening and fibrosis can occur. The adventitia is usually normal in cases without a history of rupture. Only a few reports of histologic findings in Ehlers-Danlos syndrome exist, and most show mild histologic change characterized by loss of elastic fibers and medionecrosis. The intima and adventitial layers are usually spared. Intimal tears are common and may cause intimal fibrosis, which is believed to be posthealing.
The relationship between extent of cystic medial necrosis and etiology of thoracic aortic aneurysm (TAA) has been extensive studied. It has been shown that the greatest degrees of cystic medial necrosis occur in patients with Marfan syndrome, followed by non-Marfan familial dissection. Older patients with non-hereditary thoracic aortic aneurysm (TAA) and thoracic aortic aneurysm (TAA) associated with bicuspid aortic valve have relatively small degrees of cystic medial necrosis.3 Disorganized media in areas of healed aortitis may also show proteoglycan pooling very similar to cystic medial necrosis.3,6
The histopathologic hallmark of noninflammatory thoracic aortic aneurysm (TAA) is cystic medial degeneration, or the pooling of proteoglycans (mucoid material) and pseudocysts formation in the media, accompanied by extensive loss of elastic lamellae. These changes result in the medial weakening that progresses to aneurysm, dissection, or both. A related histologic finding is so-called “medionecrosis” a finding also seen in aging aortas and in patients with hypertension. Medionecrosis, or laminar medial necrosis, is defined as coagulative necrosis of medial smooth muscle cells, resulting in loss of nuclei and collapse of the elastic lamellae,3 a finding that is not specific for any specific etiology for thoracic aortic aneurysm (TAA).
Aneurysms associated with uni- and bicuspid aortic valve disease usually show focal loss of elastic laminae and some associated intimal fibrosis, which is usually mild. MFS patients usually have severe elastic fiber degeneration of the aortic media, which can be prominent at and around the sites of gross tears. If a healing process, such as remote tear, is present, intimal thickening and fibrosis can occur. The adventitia is usually normal in cases without a history of rupture. Only a few reports of histologic findings in Ehlers-Danlos syndrome exist, and most show mild histologic change characterized by loss of elastic fibers and medionecrosis. The intima and adventitial layers are usually spared. Intimal tears are common and may cause intimal fibrosis, which is believed to be posthealing.
The relationship between extent of cystic medial necrosis and etiology of thoracic aortic aneurysm (TAA) has been extensive studied. It has been shown that the greatest degrees of cystic medial necrosis occur in patients with Marfan syndrome, followed by non-Marfan familial dissection. Older patients with non-hereditary thoracic aortic aneurysm (TAA) and thoracic aortic aneurysm (TAA) associated with bicuspid aortic valve have relatively small degrees of cystic medial necrosis.3 Disorganized media in areas of healed aortitis may also show proteoglycan pooling very similar to cystic medial necrosis.3,6
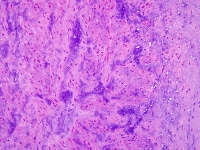
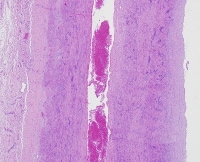
A 46-year-old woman with chest pain on exertion. Aortic dissection was diagnosed by chest radiograph. Clinical evaluation suspicious for Marfan Syndrome. Histologic sections show plane of dissection splitting the media layer in half (intima at right). Even at this magnification, one can see myxoid degeneration of the media (cystic medial necrosis).
At high magnification, the media shows a haphazard disorganization and loss of smooth muscle cells and pools of proteoglycans.
Aortitis
Takayasu disease (necrotizing aortitis) is characterized by intimal and adventitial fibrosis and inflammation, with areas of medial necrosis is varying phases of development. The histologic hallmark of Takayasu aortitis/necrotizing aortitis is multifocal medial laminar necrosis rimmed by macrophages and occasional giant cells. Loose granulomatous inflammation near necrotic areas is common. In late, healed cases, the intimal and adventitial fibrosis can be striking, and complete loss of elastic fibers in the media is appreciated. The degree of intimal fibrosis is usually greater than the cases of giant cell aortitis. The latter shows in contrast little medial destruction and minimal to no adventitial fibrosis.6,17 Calcification may be present in about 25% of cases. The adventitial fibrosis in aortitis is often accompanied by inflammation and obliteration of the adventitial vessels (endarteritis obliterans).
A 40-year-old woman with aortic insufficiency had an episode of flu-like illness, followed by right back pain. Work-up demonstrated marked dilatation of the ascending and descending aorta. This low magnification view of the ascending aorta stained with Movat Pentachrome stain show necrotizing aortitis involving mainly the media. There is a lymphocytic and focal giant cell infiltrates (not shown). The adventitia is fibrotic and shows endarteritis obliterans. There is mild intimal fibrosis. These findings are consistent with Takayasu disease.
Low magnification, Movat Pentachrome stain. There is multifocal zonal necrosis with a moth-eaten appearance of the media. The adventitia (left) and intima (right) are slightly thickened.
Giant cell aortitis in a 71-year-old female with a history of giant cell arteritis. Movat Pentachrome stain showing giant cell infiltrates within media. There is loss of smooth muscle cells, but the elastic lamellae are intact, with giant cells in the periphery.
Syphilis
Syphilitic aneurysms are similar histologically to those of Takayasu disease. Occasionally, gummatous inflammatory occurs, and spirochetal organisms may be identified by silver impregnation stains. Endoarteritis obliterans is said to be common, as in cases of noninfectious aortitis.
Bacterial or myocytic aneurysm
These subtype of infectious aneurysms demonstrate destruction of the media with acute and chronic inflammation and granulation tissue. Frequently, there is inflammation extending into adjacent structures, such as the pleura, pericardium, and lung.
Immunohistochemistry
Immunohistochemistry is of little use in the diagnosis of thoracic aortic aneurysm (TAA). In the case of noninflammatory thoracic aortic aneurysm (TAA) caused by Loeys-Dietz syndrome, positive staining for pSmad2 has been shown to be fairly specific.9 Immunophenotyping of inflammatory infiltrates in aortitis has demonstrated a wide range of inflammatory cells.17
Molecular/Genetics
Thoracic aortic aneurysms can be divided into the following 5 main categories regarding their association with genetic diseases:
- Sporadic cases with genetic imbalances and familial aggregation that may predispose the formation of thoracic aortic aneurysm (TAA)
- Cases associated with bicuspid valve disease with familial aggregation
- Marfan syndrome
- Ehlers-Danlos syndrome type IV
- Other genetic conditions predisposing to thoracic aortic aneurysm (TAA)
Many patients with aortic aneurysm and dissection do not fit any syndrome of collagen vascular disease, yet as many as 20% of those have at least one first-degree family member with a known aneurysm in the arterial tree.12Radiological screening in family members of patients presenting with aneurysms of complications thereof have identified a pool of patients with asymptomatic aortic dilatation.19
Three genomic loci for familial thoracic aortic aneurysm (TAA)s and dissections have been identified, 5q13–14, termed the TAAD1 locus, 11q23–24, the FAA1 locus, and 3p24–25, the TAAD2 locus. The latter was sequenced for the gene transforming growth factor-β receptor type 2 (TGFBR2), which may be responsible for 5% of familial thoracic aortic aneurysm (TAA). New studies have demonstrated unique polymorphisms in the THBS2 as a risk for thoracic aortic aneurysm (TAA), with some other variants being protective.20 This area of research is rapidly advancing, and many other more specific genes are expected to be identified and used in the screening of patients and family members.
Bicuspid aortic valve disease is a common congenital cardiac defect that is present in about 1% of the population. The much less common unicuspid aortic valve is also associated with thoracic aortic aneurysm (TAA). This condition happens in multiple members of the same family. Epidemiological studies have pointed an autosomal dominant inheritance, but no specific genetic aberration has been identified to date.21
Marfan syndrome has been extensive studied clinically and genetically. In the absence of surgical treatment, patients with Marfan disease have a 50 percent risk of developing aortic dissection during their lifetime. The aortic dilatation observed in MFS is the result of defects in a specific component of the elastic fiber, fibrilin-1.22 Mutations on the homologous gene, FBN1 are found on chromosome 15.
An online Marfan database contains more than 250 mutations in MFS. Mutations in the FBN2 gene, for fibrillin 2, also predispose for aortic dilatation, without a risk increase for dissection, as in patients with FBN1 mutations. A second less prevalent locus was identified in MSF-like patients at 3p24.2-p25, coded MFS2. Patients bearing this mutation have not met the criteria for MFS but seem to have a high incidence of thoracic aortic aneurysm (TAA).
The Ehlers-Danlos syndrome type IV (vascular type) is due to defects in the type III procollagen (COL3A1). It causes vascular fragility with aneurysm formation, rupture, and dissections. The aorta is involved in a small percentage, since this disease affects most often smaller arteries. Usually multiple rupture sites are found in the aorta. Other rarer genetic diseases that predispose to thoracic aortic aneurysm (TAA) are polycystic kidney disease and Ehlers-Danlos type VI (kyphoscoliotic type).
Three genomic loci for familial thoracic aortic aneurysm (TAA)s and dissections have been identified, 5q13–14, termed the TAAD1 locus, 11q23–24, the FAA1 locus, and 3p24–25, the TAAD2 locus. The latter was sequenced for the gene transforming growth factor-β receptor type 2 (TGFBR2), which may be responsible for 5% of familial thoracic aortic aneurysm (TAA). New studies have demonstrated unique polymorphisms in the THBS2 as a risk for thoracic aortic aneurysm (TAA), with some other variants being protective.20 This area of research is rapidly advancing, and many other more specific genes are expected to be identified and used in the screening of patients and family members.
Bicuspid aortic valve disease is a common congenital cardiac defect that is present in about 1% of the population. The much less common unicuspid aortic valve is also associated with thoracic aortic aneurysm (TAA). This condition happens in multiple members of the same family. Epidemiological studies have pointed an autosomal dominant inheritance, but no specific genetic aberration has been identified to date.21
Marfan syndrome has been extensive studied clinically and genetically. In the absence of surgical treatment, patients with Marfan disease have a 50 percent risk of developing aortic dissection during their lifetime. The aortic dilatation observed in MFS is the result of defects in a specific component of the elastic fiber, fibrilin-1.22 Mutations on the homologous gene, FBN1 are found on chromosome 15.
An online Marfan database contains more than 250 mutations in MFS. Mutations in the FBN2 gene, for fibrillin 2, also predispose for aortic dilatation, without a risk increase for dissection, as in patients with FBN1 mutations. A second less prevalent locus was identified in MSF-like patients at 3p24.2-p25, coded MFS2. Patients bearing this mutation have not met the criteria for MFS but seem to have a high incidence of thoracic aortic aneurysm (TAA).
The Ehlers-Danlos syndrome type IV (vascular type) is due to defects in the type III procollagen (COL3A1). It causes vascular fragility with aneurysm formation, rupture, and dissections. The aorta is involved in a small percentage, since this disease affects most often smaller arteries. Usually multiple rupture sites are found in the aorta. Other rarer genetic diseases that predispose to thoracic aortic aneurysm (TAA) are polycystic kidney disease and Ehlers-Danlos type VI (kyphoscoliotic type).
Prognosis and Predictive Factors
The prognosis of aortic aneurysms is dependent of the size of the aneurysm, which increases the risk for dissection and rupture. In patients with known Marfan syndrome, patients are followed, and elective surgery performed with an aneurysm diameter of as low as 3 cm, but generally 4-6 cm.23,24,25,26 In the case of ruptured thoracic aortic aneurysm (TAA), the prognosis is quite poor without surgical intervention in cases of type I and II dissections, and surgery is considered a medical emergency.
In the case of type III dissection, over one-half of patients survive with anti-hypertensive therapy for over one year.5The prognosis of surgery in ruptured type III dissections was dismal in the past, but newer surgical techniques and development of aortic stent grafts show hope for the future.4 Medical treatment of healed dissecting aneurysms of the distal thoracic aorta has been shown to offer longer survival than surgery.5
Of nonruptured thoracic aortic aneurysm (TAA), those with the worst prognosis are infectious, or “myocytic” aneurysm, because of the high rate of sepsis. However, surgical resection was successful with less than 25% operative mortality in one surgical series.7
Of nonruptured thoracic aortic aneurysm (TAA), those with the worst prognosis are infectious, or “myocytic” aneurysm, because of the high rate of sepsis. However, surgical resection was successful with less than 25% operative mortality in one surgical series.7
Differentials
Bicuspid aortic valve associated aortic aneurysm
Ehlers-Danlos Syndrome
Loeys-Dietz Syndrome
Marfan Syndrome
Ehlers-Danlos Syndrome
Loeys-Dietz Syndrome
Marfan Syndrome
Multimedia
 | Media file 7: Thoracic aortic aneurysm. |
 | Media file 13: Heart of a 43-year-old male sudden death case. External view of proximal aorta showing dilatation and transmural tear, after removal of blood clots from hemopericardium. |
 | Media file 14: At high magnification, the media shows a haphazard disorganization and loss of smooth muscle cells and pools of proteoglycans. |
Keywords
thoracic aortic aneurysms, dissecting aneurysms, thoracic aortic aneurysm, dissecting aneurysm, aortic aneurysm, cystic medial degeneration, bicuspid aortic valve, Marfan syndrome, dissecting aneurysm, Takayasu disease, giant cell aortitis, Loeys-Dietz syndrome, annuloaortic ectasia, aortic root dilation












0 comments:
Post a Comment